The addition of acalabrutinib to standard-of-care chemoimmunotherapy significantly extended PFS compared with standard therapy alone in a randomized study, according to press release the agent’s manufacturer.
The double-blind phase 3 ECHO trial assessed the efficacy and safety of bendamustine and rituximab (Rituxan, Genentech) with and without acalabrutinib (Calquence, AstraZeneca) — a Bruton’s tyrosine kinase inhibitor — among adults aged 65 years or older (N = 598) with previously untreated mantle cell lymphoma.

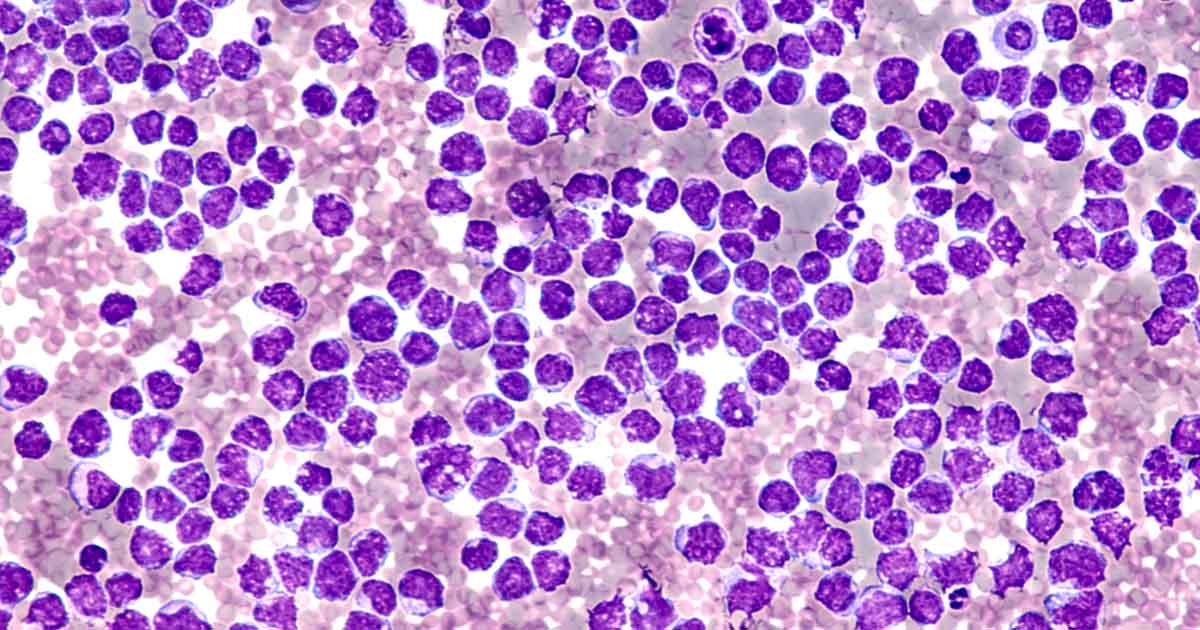
Adding acalabrutinib to standard chemoimmunotherapy significantly extended PFS for adults with mantle cell lymphoma in a randomized study. Image: Adobe Stock.
Study investigators randomly assigned participants to receive acalabrutinib or placebo administered orally twice a day, on 28-day treatment cycles, plus bendamustine on days 1 and 2 and rituximab on day 1. Following six cycles, patients then received acalabrutinib or placebo along with maintenance rituximab for 2 years, followed by acalabrutinib or placebo until disease progression.
PFS served as the study’s primary endpoint, with key secondary endpoints of OS, overall response rate, duration of response and time to response.
An interim analysis of the results showed that patients in the experimental arm of the trial demonstrated improvement in PFS compared with standard therapy.
“These positive progression-free survival results from the ECHO [phase 3 trial] could provide a new standard of care for patients with mantle cell lymphoma,” Michael Wang, MD, director of the mantle cell lymphoma program of excellence and co-director of clinical trials at The University of Texas MD Anderson Cancer Center, said in the release. “Incorporating Calquence into the first-line mantle cell lymphoma setting would give many more patients the opportunity to benefit from the robust efficacy and strong safety profile we’ve seen with this medicine.”
Researchers noted similar safety and tolerability data consistent with the known safety profile of acalabrutinib, with no new safety signals reported. Data from the analysis will be presented at an upcoming medical conference, according to the release.