Children and adolescents diagnosed with high blood pressure have double the risk of major cardiovascular problems as adults, a new study that followed them into their 20s and 30s reports.
It’s another example of a serious disease striking people at younger ages than in previous generations and should serve as a call to action for routine blood pressure screening in primary care, Rahul Chanchlani, the senior author of the new study, told STAT.
“These are those children where a physician actually took the blood pressure and labeled them with hypertension. Imagine the vast majority of the pediatric population where they’re not even checking blood pressure,” said Chanchlani, associate professor of pediatric nephrology at McMaster Children’s Hospital in Hamilton, Ont. Citing hypertension’s reputation as a “silent killer,” he said, “The majority of these children or adults have no signs or symptoms, so unless you check it, you’re going to miss it.”
The new paper, appearing Monday in JAMA Pediatrics, delves into outcomes from diagnosed hypertension, tracking more than 25,000 Canadian young people who were 3 to 17 years old when the study started in 1996, comparing them to more than 128,000 children and adolescents without known high blood pressure. Based on medical records and adjusted for possibly confounding factors, they found that by 2021, hypertension diagnosed in childhood was associated with a higher likelihood (6% vs. 3%) of having a stroke, being hospitalized for a heart attack or unstable angina, and developing congestive heart failure.
They did not discern a link to deaths from cardiovascular causes, but Chanchlani said major cardiac events would still reduce quality of life. “These are people still in their 20s or maybe early 30s,” he said. “This is pretty young for a heart attack.”
The fact that pediatric hypertension was associated with risk for cardiovascular disease didn’t surprise Amanda Marma Perak, a pediatric preventive cardiologist at Lurie Children’s Hospital in Chicago who works with kids and teens who have risk factors for cardiovascular diseases, including high cholesterol, high blood pressure, and a family history of heart disease. Also an assistant professor of pediatric cardiology and preventive medicine at Northwestern University Feinberg School of Medicine, she was not involved in the JAMA Pediatrics study.
Previous research has linked high blood pressure to signs of trouble, she said, based on imaging that peers into the heart and blood vessels, but the new paper goes further.
“It provides evidence to directly link pediatric hypertension to premature CV events — which is hard to come by given the relatively long period between childhood and CV events (which means you need really good, really long duration follow-up to find a link),” she told STAT via email. “This paper helps add to the evidence by leveraging a very large, national database with very high rates of follow-up for many years.”
The people at higher cardiovascular risk call to mind adults under 45 whose deaths from heart failure are rising, reversing a decline that began 1999, as a recent study documented. People under 50 are developing colorectal cancer, before an age when previous standards had called for screening.
Guidelines for checking blood pressure in children vary. Medical societies such as the American Academy of Pediatrics, the European Society of Hypertension, and Hypertension Canada do recommend annual blood pressure screening for healthy children over 3 years old, but two groups with influence on practice do not: the United States Preventative Services Task Force and the United Kingdom National Screening Committee. In 2020 the USPSTF called current evidence “insufficient” to assess the benefits and harms of screening for high blood pressure in children and adolescents.
Michael Silverstein, USPSTF vice president, said in a statement on Friday the task force welcomes new research that could potentially inform its recommendations.
“When we published our latest recommendation on screening children for high blood pressure in 2020, the latest science clearly showed there was not yet sufficient evidence to demonstrate whether screening for blood pressure in kids leads to improved cardiovascular health,” he said. Asked if the topic would be revisited, he said “we regularly re-review our guidance to ensure it reflects the most up-to-date scientific evidence, and we will be eager to look at any relevant new studies as part of that process.”
While blood pressure screening for children ticked up in Canada after new guidelines from the Canadian and American medical societies were published in 2016 and 2017, consistent follow-up in primary care practices faltered after about six months, a JAMA Network Open study led by Chanchlani reported earlier this year. The prevalence of hypertension in adults in Canada is about 23%, lower than the 30% found in the United States, a 2019 study said, defined by blood pressure readings above 130/80.
Chanchlani and his co-authors call pediatric hypertension an epidemic, one whose prevalence has soared fivefold over the last three decades. He blames a lack of awareness, among both doctors and families, of the need to look for a well-known risk factor in adults.
“Identification is the first step,” Perak said about blood pressure measurement. “In the clinics, we need consistent, reliable readings that health care practitioners trust. Protocols for measuring accurately can be tricky and time consuming.”
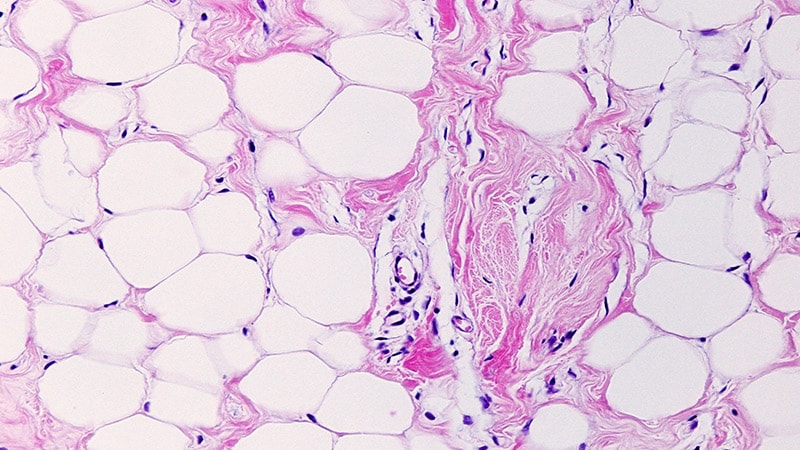
In children and adults, hypertension damages vessels with its sustained pounding of arteries and veins. Blood pressure normally subsides after climbing stairs or watching a horror movie, but if it stays consistently high, under-the-radar damage can build for years, harming the brain, heart, and kidneys. It’s worsened by lifestyles marked by more high-salt junk food and screen time but less sleep and exercise.
There are treatments for children that work — medications and lifestyle changes — if their high blood pressure is detected.
“We showed that children who had high blood pressure had a higher risk of an enlarged heart, compromised blood vessels,” Chanchlani said about previous research. “When it is treated, it is absolutely reversible.”
Perak urged more research on pediatric hypertension to find more answers.
“We know that medications and lifestyle changes can bring BP down in childhood at least in the short term,” she said, “but we need to know more about whether/how/when/which of these interventions can best reduce risk of actual CV events.”
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies. Our financial supporters are not involved in any decisions about our journalism.