An article published in the journal Best Practice & Research Clinical Gastroenterology provides an in-depth overview of the Western diet’s impact on modulating gut microbiota and gut barrier functionality and subsequently increasing the risk of non-communicable chronic diseases.
Study: The microbiome-driven impact of Western diet in the development of noncommunicable chronic disorders
Background
The Western diet contains high amounts of saturated fats, refined sugars and grains, salt, sweeteners, processed red meat, high-fat dairy products, low amounts of fruits and vegetables, fiber-rich foods, whole grains, fish, nuts, and seeds.
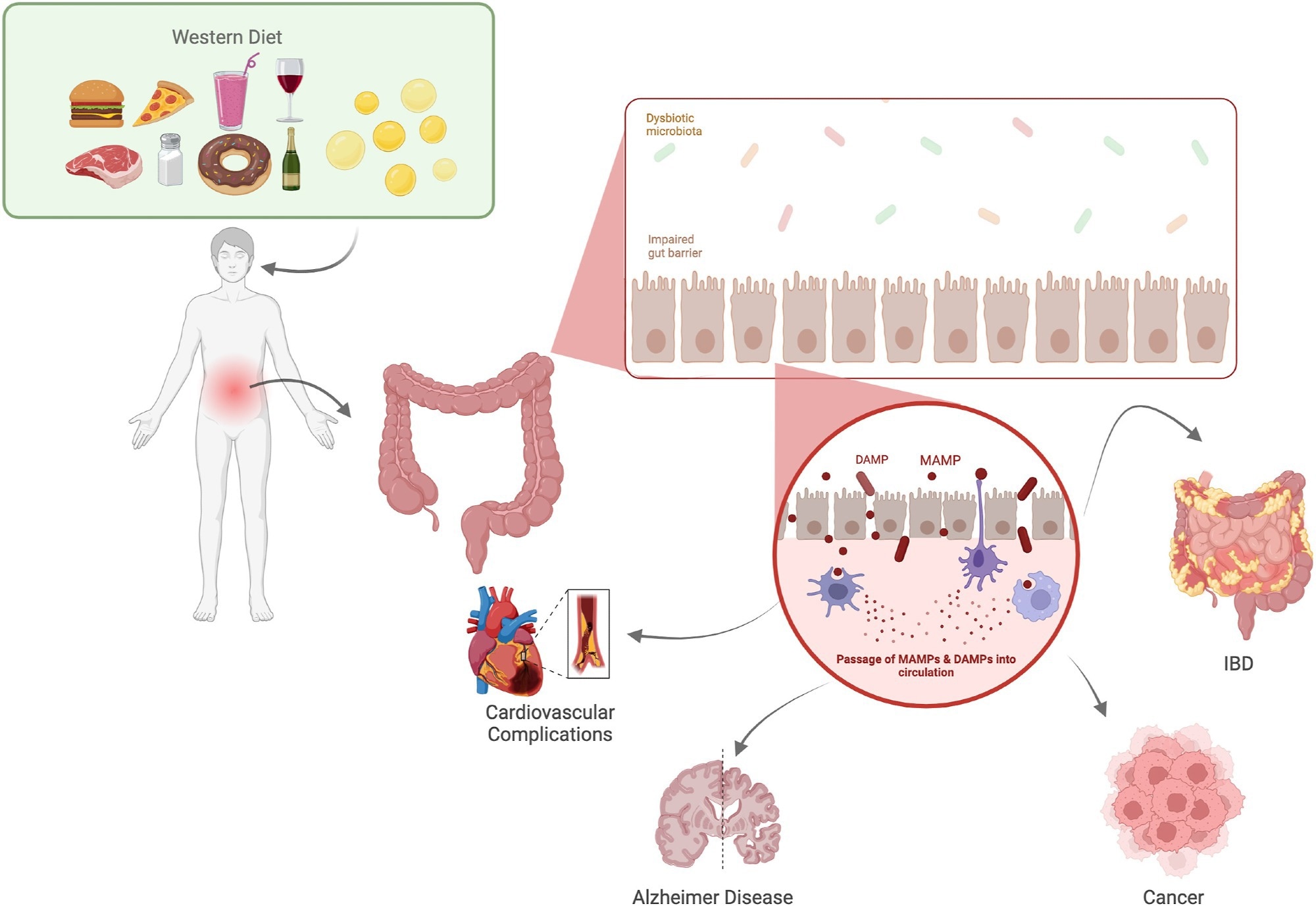
The Industrial Revolution gradually increased the predominance of Western diet worldwide for nearly 100 years. Consumption of a Western diet, which is low in vital nutrients, has been linked to the development of a chronic, low-inflammatory state and impairment of gut microbiota, which are major hallmarks of non-communicable chronic diseases.
Non-communicable diseases are a group of health conditions that are not primarily caused by an acute infection. These conditions include cardiovascular disease, diabetes, metabolic syndrome, irritable bowel syndrome, inflammatory bowel disease, chronic lung disease, neurodegenerative diseases, and neuropsychiatric diseases.
Western diet and gut microbiota
Diet contributes significantly to shaping the composition and functionality of gut microbiota, a complex microbial ecosystem that plays vital roles in human physiology and pathology.
The nutrient components present in the Western diet are responsible for altering gut microbiota composition. Refined oils in the Western diet have been found to reduce the abundance of beneficial bacteria and increase the abundance of pathogenic bacteria in the intestine.
Western diet contains high omega-6 polyunsaturated fatty acids (PUFAs) and low omega-3 PUFAs. An increased omega-6/omega-3 PUFA has been found to induce pro-inflammatory mediators and suppress anti-inflammatory mediators.
Other vital components of the Western diet, including red meat, refined sugar, salt, and artificial sweeteners, have been shown to cause gut microbiota imbalance (dysbiosis), characterized by reduced beneficial bacterial population and increased pathogenic bacterial population.
Western diet and gut barrier
The primary functions of the gut barrier are to facilitate the absorption of essential nutrients and fluids and to prevent the entry of harmful substances.
Western diet has been found to affect the structure and function of the gut barrier in multiple ways. High amounts of saturated fats present in this have been found to reduce the expressions of tight junction proteins and barrier-forming proteins through the modulation of gut microbiota.
Saturated fats have also been found to increase bile acid release, which in turn increases gut permeability. Similarly, low fiber content in the Western diet has been found to cause a shifting of bacterial metabolism, disrupting the muco-epithelial barrier and induction of gut permeability.
A low-fiber diet-induced reduced production of short-chain fatty acids by gut microbiota has been found to suppress the production of mucus, antimicrobial proteins, and regulatory T cells, leading to an alteration in gut barrier permeability.
Western diet and non-communicable chronic diseases
Western diet-induced gut microbiota imbalance, gut barrier dysfunction, and increased barrier permeability can release toxic bacterial metabolites (lipopolysaccharides) into the bloodstream and subsequent induction of systemic inflammation. Western diet-induced promotion of chronic, low-grade inflammation can increase the risk of various non-communicable chronic diseases.
The recognition of lipopolysaccharides (LPS) by pattern recognition receptors (toll-like receptor 4; TLR4) leads to increased expression of pro-inflammatory cytokines, increased gut permeability, and promotion of local and systemic inflammation.
Saturated fats in the Western diet can directly stimulate the NF-kB pathway via TLR4, increase mitochondrial fatty acid oxidation, and increase reactive oxygen species (ROS) production, which collectively lead to increased inflammation.
Western diet is associated with increased production of trimethylamine N-oxide (TMAO), which increases the risk of cardiovascular disease, diabetes, and obesity. Gut microbiota imbalance caused by a Western diet has been found to increase functional capacity to harvest energy and produce cardio-toxic chemicals, which collectively increase the risk of obesity and metabolic syndrome.
An altered gut microbiota, characterized by reduced microbial diversity, stability, butyrate, and an increased abundance of methane-producing bacteria, has been observed in patients with irritable bowel syndrome.
High intake of red meat, processed foods, refined sugar, and saturated fat has been found to increase the risk of ulcerative colitis and irritable bowel syndrome.
High intake of saturated fat and refined sugar has been found to steadily reduce hippocampus-dependent learning and memory and increase inflammation in the hippocampus and amygdala. An association has also been observed between Western diet intake and increased accumulation of Alzheimer’s disease biomarkers (beta-amyloid) in the brain.
Western diet has been found to increase depression risk through nutrient-microglia and gut-immune interactions. An alteration in gut microbiota composition and diversity has been observed in patients with major depressive disorder.
Potentials for therapeutics
A healthy diet contributes significantly to a healthy gut microbiota. The Mediterranean diet, a rich source of dietary fibers, mono- and polyunsaturated fatty acids, polyphenols, and other vital nutrients, has been found to significantly reduce the risk of non-communicable chronic diseases through maintaining a healthy gut microbiota.
Besides dietary modifications, other interventions that have shown promising outcomes in maintaining gut health include physical exercise and regulation of circadian clocks.