An alarming lack of compliance with assessments to prevent ophthalmologic and neuropathic complications associated with diabetes has been detected in nine countries in Latin America and the Caribbean. Only three territories (Chile, Brazil, and the British Virgin Islands) had more than 50% of patients with diabetes who had received an eye examination in the previous 2 years. Meanwhile, the rate of foot assessments was below 41% in all countries during the previous year.
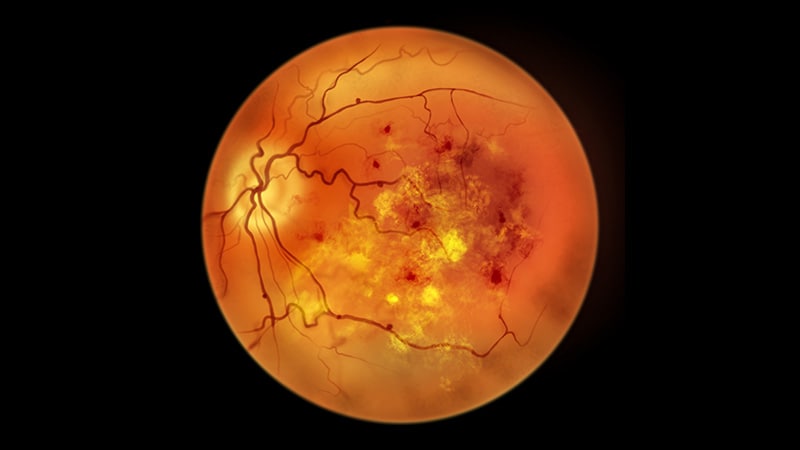
“These numbers are concerning. Patients with diabetes are at risk of developing retinopathy and neuropathy, which can lead to amputations. Without prevention, this risk increases. The results suggest that despite clear recommendations in clinical guidelines, they are not being followed,” Rodrigo Carrillo Larco, MD, PhD, an epidemiologist and researcher at the Emory University School of Public Health in Atlanta, and lead author of the study published in Primary Care Diabetes, told the Medscape Spanish edition.
The evidence comes from a cross-sectional study that analyzed data from nine national surveys (Argentina, the Bahamas, Bolivia, Chile, Brazil, Ecuador, the British Virgin Islands, Mexico, and Uruguay). This approach allowed for the grouping of 7435 adults with diabetes aged 25-64 years.
Due to survey characteristics, it was not feasible to determine whether patients had type 1 or type 2 diabetes. But participants’ variables such as age, body mass index, hypertension, diabetes treatments, duration of living with diabetes, and family history of diabetes were recorded.
Due to disparities in the survey timeframe, the authors cautioned against comparing the findings between countries. Instead, they urged clinicians to use the results to describe the current situation in each country.
Following this caveat, the study revealed that only Chile (64%), the British Virgin Islands (58%), and Brazil (55%) surpassed the 50% threshold of patients with diabetes undergoing ophthalmologic evaluation. On the other end, Bolivia (22%), Ecuador (22%), and Mexico (15%) did not exceed 30% of examined patients, while Argentina, Bahamas, and Uruguay fell within an intermediate range.
Older patients (age, 55-64 years) and those under insulin or oral hypoglycemic control were more likely to have undergone an ophthalmologic evaluation.
The results were not better when foot assessments were analyzed. No country in the study examined more than 50% of patients with diabetes. Those that came closest were Chile (41%), the Bahamas (37%), and Brazil (32%). But the remaining six countries (Argentina, Bolivia, Ecuador, Mexico, Uruguay, and the British Virgin Islands) did not surpass the 30% threshold. Once again, the percentages favored older individuals and those under insulin or oral hypoglycemic treatment.
“The study sets the groundwork for understanding what happens in diabetes with preventive measures, especially secondary and tertiary ones. Understanding that levels are low can help propose appropriate management alternatives,” said Antonio Bernabé Ortiz, MD, PhD, MPH, lead author and a public health physician, epidemiologist, and researcher at the Scientific University of the South, Lima, Peru.
Measure to Improve
“This is a very interesting study, and from my point of view, the research is relevant because it quantifies the reality of preventing chronic complications that strongly impact the quality of life of people with diabetes,” said Carolina Gómez Martin, MD, a diabetologist and codirector of the Cendia care center in the province of Entre Ríos, Argentina, and a member of the board of directors of the Argentine Diabetes Society.
“You can’t improve what you don’t measure, and having concrete data is the first step in designing and implementing strategies to optimize the quality of care and reduce the dreaded complications of diabetes,” she added. Gómez Martin did not participate in the study.
The study did not explore the reasons behind the poor results obtained in the region.
Carrillo Larco pointed out that factors inherent to the patient would also influence the rate of screening, such as lack of knowledge, minimization of diabetes complications, or lack of empowerment to demand a complete and periodic evaluation.
Regarding healthcare systems, he highlighted the lack of access to care, limited consultation times, and low availability of specialized resources for preventive consultations.
On the other hand, he noted that the study could promote initiatives that encourage screening and prevention of complications. Likewise, he considered that based on this research, “there is clear evidence that there is ample room for improvement, and the results of this work can help design or strengthen health interventions and policies.”
Gómez Martin agreed that the health systems in the region have much to achieve despite the countries’ limited resources. “At this point, I believe that the development of public policies that guide the available resources to primary care, education, and prevention of complications is fundamental. This will improve the quality of life of people with diabetes and reduce the high costs of treating advanced complications,” she said.
Clinicians and Technologies
Carrillo Larco hopes that these numbers will help physicians care for patients with diabetes. Physicians are the ones who must motivate and reinforce the performance of these evaluations, prescribe them more often, discuss their implications and benefits, empower patients to request them, and work to ensure they are carried out in their institutions, he said.
The main message of the study is that “we must put our greatest effort into following the guidelines for the detection and prevention of complications that have such a negative impact on people with diabetes and continue to educate our patients for awareness and self-care,” said Gómez Martin.
Public policies, rather than individual actions, will be able to change this reality, she added.
The study results suggest a need for innovative research in this area, especially in contexts of limited resources. The first thing needed is to know what a patient with diabetes knows about their disease and the complications it generates, said Bernabé Ortiz. “This would help propose educational strategies using technology, for example, chatbots. Cocreation techniques with the patients themselves can also be useful to understand what they need from the system.”
Gómez Martin considered that technology provides tools that would allow cost reduction, scaling of prevention programs, bringing people closer to health providers through various communication channels (such as text messages, video consultations, or sending educational materials), or implementing retinopathy prevention programs in places where no ophthalmologists are available. “This field is vast and advancing rapidly. Health teams and decision-makers have the responsibility to use these tools for the benefit of all people living with diabetes,” she said.
“Studying the implementation of these or other strategies and how they are received and used by patients with diabetes is imperative,” said Bernabé Ortiz.
“The guidelines exist, so why aren’t they implemented? What are the barriers to such implementation? Is having a guideline all that is needed? These are all questions that still have no answer and may depend on the context in which they are asked,” he concluded.
Carrillo Larco, Bernabé Ortiz, and Gómez Martin declared no relevant financial conflicts of interest.
This story was translated from the Medscape Spanish edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.