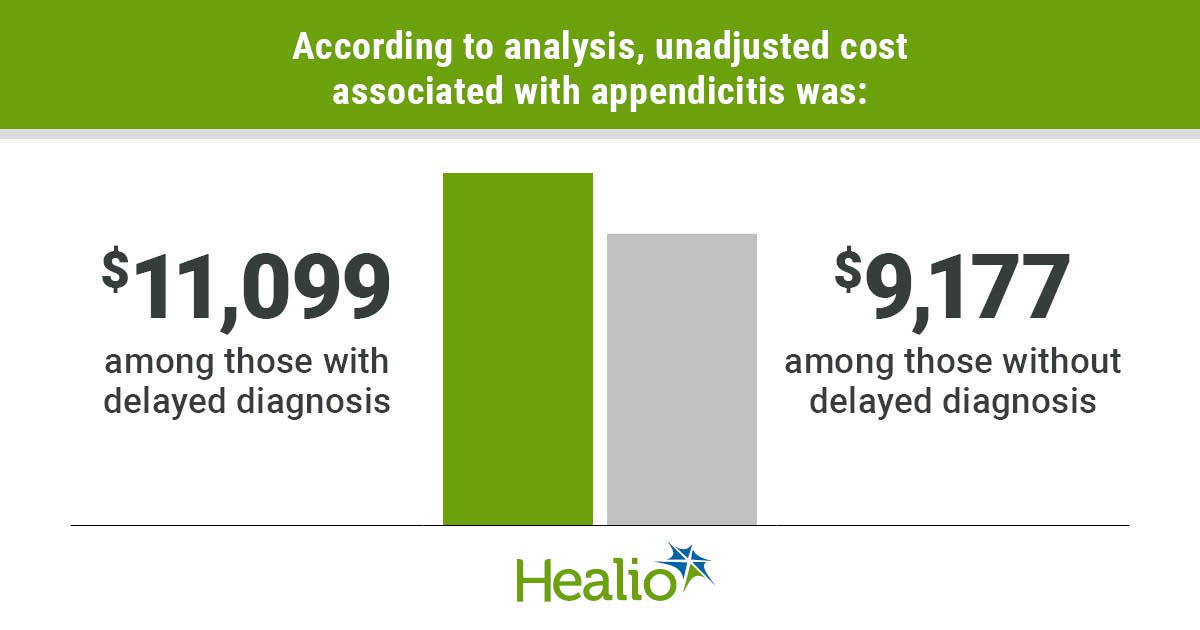
Key takeaways:
- Patients with a delayed diagnosis had an unadjusted median cost of $11,099 vs. $9,177 for patients with a non-delayed diagnosis.
- Non-Hispanic Black patients with a delayed diagnosis had a higher median cost.
A delayed diagnosis of appendicitis was associated with an increase in hospital care costs in a cohort of adults who underwent appendectomy, particularly among non-Hispanic Black patients, according to data in JAMA Network Open.
“Delayed diagnoses have resulted in increased appendectomy length of stay and 30-day readmissions,” Dinushi A. Kulasekere, BS, of Northwestern University Feinberg School of Medicine, and colleagues wrote. “And while delayed diagnosis has been commonly observed among non-Hispanic Black patients, hospitals that serve a higher proportion of non-Hispanic Black patients have received lower payer reimbursement for care, exacerbating disparities.”

Data derived from: Kulasekere DA, et al. JAMA Netw Open. 2024;doi:10.1001/jamanetworkopen.2024.6721.
They continued: “However, it is unclear whether increased costs were associated with delayed appendicitis diagnosis or operational delays to appendectomy. There is a research gap in whether delayed appendicitis diagnosis is associated with increased appendicitis hospital care costs.”
Using the Healthcare Cost and Utilization Project State Inpatient and Emergency Department databases, researchers identified 76,183 patients aged 18 to 64 years (51.1% women; 24.1% aged 25-34 years) who underwent surgical treatment for appendicitis in five states from 2016 to 2017.
Most patients were non-Hispanic white (61.6%), followed by Hispanic (18.5%), non-Hispanic Black (10.8%) and Asian or Pacific Islander (2.9%). More than half of patients (62.8%) were privately insured, while 19.9% and 4% were covered by Medicaid and Medicare disability, respectively.
Overall, 2.7% of patients had a delayed appendicitis diagnosis, of whom 15.6% identified as non-Hispanic Black. Among all racial and ethnic categories, non-Hispanic Black patients had the highest rate of delayed diagnosis (3.9%) vs. non-Hispanic white (2.6%), Hispanic (2.5%) and Asian (2%) patients.
According to analysis, patients with a delayed diagnosis had significantly higher unadjusted costs (median, $11,099) compared with patients without a delayed diagnosis (median, $9,177). Further, patients with a delayed diagnosis had 1.23-times (95% CI, 1.16-1.28) higher adjusted costs of hospital care, with a mean marginal cost of $2,712 (95% CI, 2,083-3,342).
After adjusting for delayed diagnosis, non-Hispanic Black patients had 1.22-times (95% CI, 1.17-1.28) higher adjusted costs compared with non-Hispanic white patients.
“In this cohort study, delayed diagnosis was associated with increased appendicitis hospital care costs,” Kulasekere and colleagues wrote. “Appendicitis hospital care costs were higher among hospitals that served greater than 75% Black and Hispanic patients compared with hospitals that served less than 25% Black and Hispanic patients.”
They concluded: “These results suggest that delayed diagnosis may be a more equitable quality metric for payers to construct value-based reimbursement policies, one that would reward high-quality performance at hospitals that treat a greater proportion of patients from racial and ethnic minority groups, which would in turn help offset some of the cost burden instead of differentially penalizing them and worsening health system inequities.”