In a recent review published in the journal Nature Reviews Immunology, researchers discussed the limitations of current influenza vaccines and the potential for future vaccines to induce both T-cell responses and antibodies for enhanced protection. They examined the strategies to develop influenza vaccines with broad strain specificity and long-term efficacy, covering protection requirements, immune response evaluation, expected outcomes, and financial considerations.
Study: Opportunities and challenges for T cell-based influenza vaccines. Image Credit: CI Photos / Shutterstock
Background
Influenza, a longstanding public health challenge, has caused significant morbidity and mortality worldwide, with annual death tolls up to 650,000. The coronavirus disease 2019 (COVID-19) pandemic temporarily lowered influenza activity, but as restrictions ease, cases are resurging. Vaccination remains pivotal in mitigating influenza’s impact, yet existing vaccines have limitations, including variable effectiveness. Prioritizing vaccination for high-risk groups is crucial. The present review highlights the importance of ongoing influenza prevention efforts amid evolving public health landscapes. It explores enhancing traditional influenza vaccines by eliciting broader and more durable immune responses across multiple influenza strains and seasons.
Current vaccines
The past decade has seen advancements in influenza vaccine technologies, including quadrivalent formulations and non-egg-based production methods, aiming to improve strain specificity and durability. Antibody-focused strategies dominate, but recent research suggests inducing broadly reactive antibodies targeting hemagglutinin stem regions and neuraminidase for universal influenza vaccines. Effectiveness varies yearly, with recent high-dose, adjuvanted, and novel cell-based vaccines showing modest improvements. However, even the best influenza vaccines fall short compared to highly efficacious vaccines for other pathogens, underscoring the need for further research and innovation.
Factors limiting the effectiveness of influenza vaccines
Influenza vaccine performance is challenged by antigenic variation, original antigenic sin, high levels of pre-existing immunity in the population, and a focus on antibody responses rather than broader immune activation. Antigenic shifts in circulating viruses, coupled with pre-existing immunity, reduce vaccine effectiveness. Original antigenic sin may limit vaccine efficacy by preferentially boosting cross-reactive antibodies. Moreover, the predominance of antibody-based vaccines may not fully replicate natural immune responses, suggesting a need for innovative strategies to induce more comprehensive immunity, including CD4+ (cluster of differentiation 4) and CD8+ T-cell responses.
T-cells in influenza virus infection
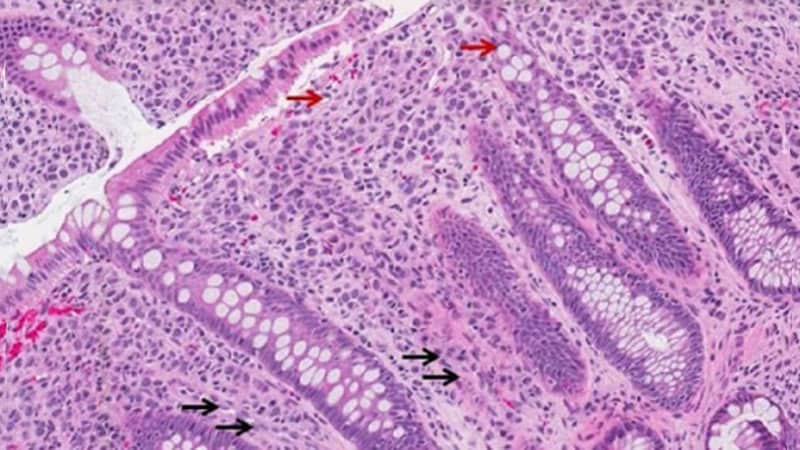
T-cells play a crucial role in influenza virus immunity, contributing to protection through cytotoxicity, inflammatory cytokine release, and support for antibody responses. CD4+ T-cells, particularly TH1 cells, are essential for promoting antibody responses and clearing infected cells, while CD8+ cytotoxic T lymphocytes (CTLs) target and kill infected cells. Additionally, CD4+ T helper cells support B-cell responses, and resident memory T-cells (TRM) provide rapid resistance to local infection, potentially intercepting early infectious events. Despite challenges such as antigenic variation and immune memory, T-cell responses remain vital for influenza vaccine efficacy and could be harnessed for improved protection strategies.
Do human T-cells protect against influenza?
Multiple studies in both mouse models and humans demonstrate the protective role of T-cells, particularly CD8+ and CD4+ T cells, against influenza virus infection. While T-cell responses may not prevent infection, they reduce symptomatic illness and contribute to viral clearance. Studies involving human challenge with influenza viruses show correlations between pre-existing T-cell responses and reduced virus shedding and symptom severity. Observational studies during the 2009 H1N1 pandemic and subsequent seasons further support the protective effects of T-cell immunity against symptomatic influenza illness. However, the potential role of non-neutralizing antibodies in mediating protection alongside T-cell responses warrants further investigation. Overall, these findings underscore the importance of T-cell-mediated immunity in influenza virus defense.
Vaccine design and delivery platform
Hemagglutinin in vaccines generates neutralizing antibodies, and neuraminidase induces non-neutralizing antibodies. Adjuvants enhance immune function. Vaccine delivery routes influence systemic or local responses. Messenger ribonucleic acid (mRNA) vaccines induce CD4+ and CD8+ T cells. Viral vectors elicit CD8+ T-cell responses. Nanoparticles promote tissue-resident memory T-cell priming. Optimizing these factors can enhance influenza vaccine efficacy by stimulating appropriate immune responses.
Designing vaccines to induce T-cells
Recent trials of T-cell-inducing influenza vaccines yielded mixed results. While OVX836 showed 84% protection, FLU-v demonstrated efficacy with a single dose, and M-001 showed no efficacy. Concerns include narrow T-cell responses. Safety was good, highlighting the need for more extensive phase IIb or III trials. Criteria for success of T-cell vaccines require careful consideration.
Designing vaccines to induce T-cells and antibodies
Combining T-cell-inducing vaccines with antibody-inducing ones enhances protection, replicating the synergistic response observed in natural infections. This approach is currently under investigation in vaccine development against COVID-19 and acquired immunodeficiency syndrome (AIDS).
Challenges to developing T-cell-inducing vaccines
Measuring immune responses in vaccine development poses challenges due to the complexity of correlating protective mechanisms. Evaluating T-cell responses is particularly intricate, requiring sophisticated assays and considerations of compartmentalization, while assessing success relies on endpoints that may not fully capture T-cell-mediated protection, emphasizing the need for comprehensive evaluation methods in clinical trials.
Conclusion
In conclusion, efforts to improve influenza vaccines, including T-cell-inducing strategies, are crucial given their modest efficacy compared to other vaccines. Innovative approaches, bolstered by lessons from COVID-19, hold promise for addressing the ongoing burden of influenza, necessitating increased research, investment, and a redefined approach to vaccine development and evaluation.