Key takeaways:
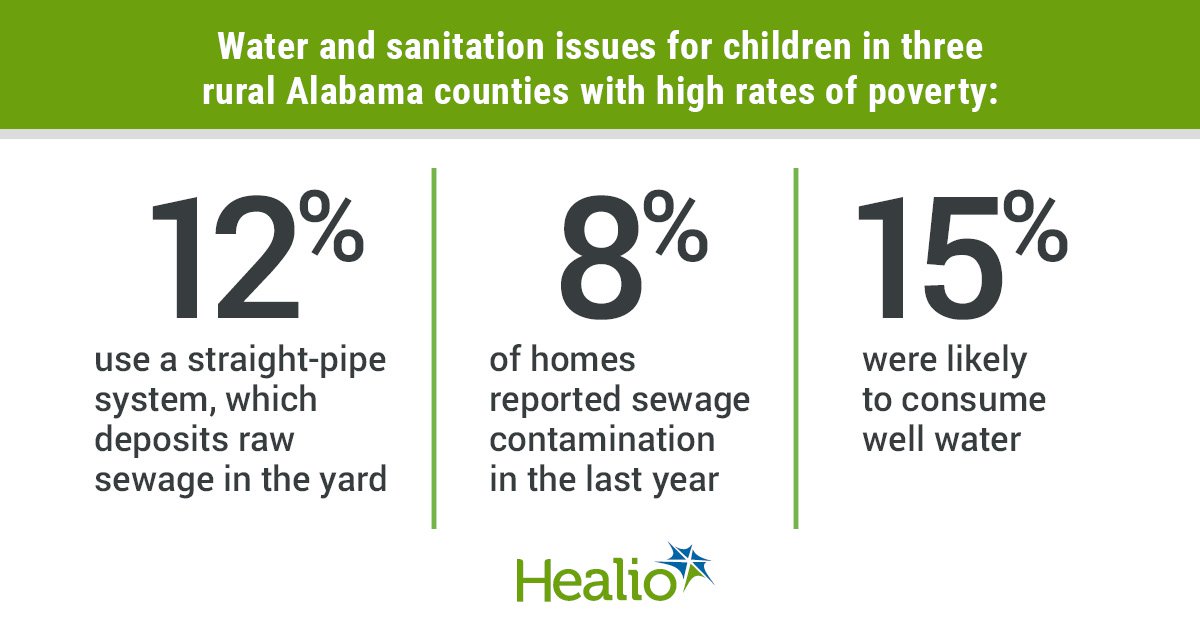
- Most children in three rural Alabama counties live in a house not connected to a sewer system.
- Nearly 1 in 10 homes in these counties reported sewage contamination.
Most children in three rural Alabama counties live without connections to centralized sewer systems, placing them at risk for certain infections, according to a study published in Pediatrics.
The study identified widespread lack of access to safe water and sanitation in these counties, and a low awareness among providers about sanitation-related health concerns.
Data derived from Poole CL, et al. Pediatrics.2024;doi:10.1542/peds.2023-063981.
The findings were part of a large multiphase project that was originally initiated to evaluate the presence of hookworm and related parasites in the Alabama Black Belt region, one of the researchers told Healio.
Originally named for the color of its soil, the Alabama Black Belt “refers to a region of southern Alabama that is largely rural and has experienced decades of economic decline and out migration,” the researchers wrote.
“Environmental engineers had been documenting the pervasive failures of household sanitation in the region but the first suggestion of impact on community health was published in 2017, suggesting that hookworm remained endemic in the region,” Claudette Poole, MD, assistant professor and associate program director of the pediatric infectious diseases fellowship program at the University of Alabama at Birmingham Heersink School of Medicine, told Healio.
Poole and colleagues used a community-based participatory research methodology, collecting data from self-administered surveys conducted in Alabama’s Lowndes, Perry and Wilcox counties, which the 2020 U.S. census determined were 70% populated by African Americans, with 37% of children living in poverty. They also conducted a survey of health providers from local federally qualified health centers and from a quiz of providers enrolled in an online sanitation health course.
According to 771 surveys completed by eligible participants from 442 households between Dec. 12, 2019, and Aug. 10, 2022, 48% of respondents living in Perry County reported a sewer connection, the highest rate. Use of septic tanks was reported by 57% of respondents in Lowndes County and 49% in Wilcox County.
Among all survey respondents, 12% reported use of “straight-pipes,” a method of discharging untreated sewage to the ground outside the home, and 8% reported sewage contamination of their home property in the past year. Additionally, 15% of respondents were likely to use well water.
“The absence of intestinal parasitic diseases was somewhat surprising given the widespread and pervasiveness of environmental sewage contamination,” Poole said. “Another surprising finding was the number of homes that geographically are within the limits of being able to connect to centralized sewer facilities [but] are not connected and discharge the household wastewater directly to the ground surface.”
In surveys of health care practitioners, only five of the 11 medical practices surveyed included routine screening for water and sanitation failures or associated infections, and regional health care providers had limited knowledge of soil-transmitted helminthiasis, with only 54% of respondents passing a five-question online course on the topic, according to Poole and colleagues.
“The general lack of health provider knowledge and awareness of the issue was not surprising due to the prevailing narrative of universal access to safe water and sanitation in the United States, and that infections such as hookworm were no longer endemic in the United States,” Poole said.
Poole called it a “complicated issue that has evolved through how we fund and regulate water and wastewater infrastructure in the United States,” and noted that she is interested in learning how inadequacies of water and wastewater infrastructure impact public health in the U.S. specifically.
“The presumption of access to safe drinking water and adequate household sanitation is not correct, as there remains communities whose water and sanitation infrastructure are inadequate,” Poole said. “Health providers need to be aware of these environmental conditions, as hygiene and safe water are fundamental to health, would change risk assessment for certain procedures and home care instructions, and should alert providers to consider screening for fecal and waterborne pathogens.”