Key takeaways:
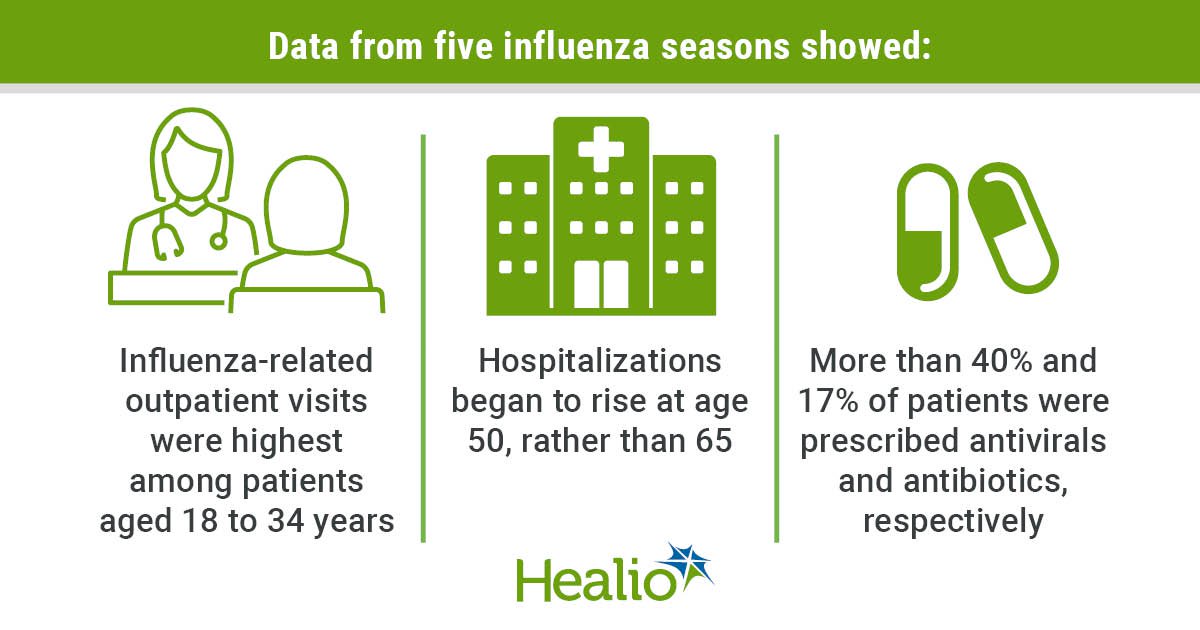
- Hospitalizations began to rise in 50-year-old patients, rather than those 65 and older.
- Influenza-related outpatient visits were highest among patients aged 18 to 34 years.
Influenza-related hospitalization rates begin to increase in patients at a younger age than previously assumed, indicating that prevention strategies should be encouraged for younger patients, researchers found.
“The study was prompted by limited existing research on how the burden of influenza varies with increasing age,” Ian McGovern, MPH, associate director of the Center of Outcomes Research and Epidemiology at CSL Seqirus, told Healio.

Data derived from McGovern I, et al. Clin Infect Dis. 2024;doi:10.1093/cid/ciae180.
“While the focus of influenza interventions and public health initiatives in adults is often among those over the age of 65 or with specific risk factors for influenza, there is evidence that individuals between the ages of 50 and 64 are also at an elevated risk from influenza infection and severe outcomes following infection,” McGovern said.
To evaluate how the incidence of influenza-related health care encounters varies among adult age groups, the researchers retrospectively evaluated adult patients across five seasons from 2015 to 2020. Electronic medical records linked to pharmacy and medical claims were then used to establish patient characteristics and outcomes.
Overall, the study showed that the incidence of influenza-related outpatient visits was highest among people aged 18 to 34 years and declined with increasing age, with ED visits also being elevated for patients of this age group. ED visits remained stable among patients aged 35 through 60 years but rapidly increased after 60 years.
The study also showed that hospitalization incidence remained stable until about 50 years of age, when it then began to increase. McGovern said that this trend suggests a “gradual shift” in the burden of disease toward younger age groups than previously recognized. He added that this could impact how manufacturers and health care providers should approach influenza protection.
“While influenza vaccination is recommended for all eligible individuals 6 months of age and older in the U.S., there are substantial differences in coverage between age groups,” McGovern said. “Notably, older adults 65 years of age or older receive the most burden of influenza as well as the most vaccination effort, with an influenza coverage of 69.7% compared with 50.1% for individuals 50 to 64 years and 35.2% for those 18 to 49 years.”
He added that this shows there is an opportunity to “ramp up education to younger adults to encourage vaccination and increase rates so that they more closely reflect those of adults 65 years of age or older.”
Additional findings from the study showed that among patients with an influenza-related outpatient visit, 1.6% to 2.8% of those 18 to 49 years old, 3.4% to 4.5% of those 50 to 64 years old and 5.5% to 7.9% of those 65 years and older had a pneumonia-related medical encounter within 2 weeks.
Across all five seasons, 40.8% and 17.% of patients were prescribed antivirals and antibiotics, respectively, after an influenza-related medical encounter. Antivirals were more commonly prescribed to patients aged 18 to 64 years compared with older adults, whereas antibiotics were more commonly prescribed to those aged 50 years and older.
McGovern said that these findings call for broader reconsideration of at-risk populations.
“To help reduce influenza-related hospitalizations for adults aged 50 and above, strategies to encourage influenza vaccination should expand their focus to include people aged 50 to 64 years, in addition to the ongoing emphasis on those who are 65 years and older,” he said. “[The findings also] emphasizes the importance of influenza vaccination as a critical tool in combating not only the direct burden of influenza but also the risk of antimicrobial resistance driven by the frequent prescription of antivirals and antibiotics following influenza infections.”