TOPLINE:
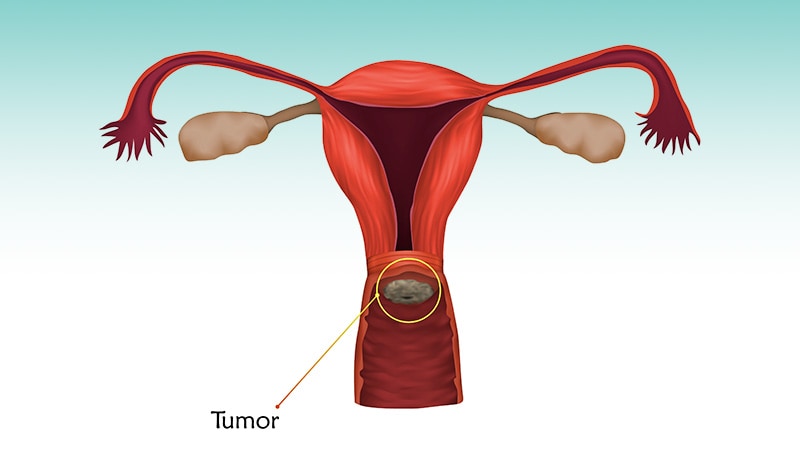
A hypofractionated intensity-modulated radiotherapy (IMRT) may be safe and well-tolerated in women with cervical cancer undergoing pelvic irradiation with concurrent chemotherapy following surgical resection, results from the phase 2 POHIM-CCRT trial suggested.
METHODOLOGY:
- To date, no studies have assessed the treatment outcomes and toxic effects of hypofractionated IMRT following radical hysterectomy in patients with cervical cancer undergoing curative radiotherapy.
- The team analyzed outcomes from 79 patients undergoing hypofractionated IMRT for cervical cancer after radical hysterectomy and pelvic lymph node dissection.
- Patients were a median age of 48; 29.5% had stage IB to IIA disease, another 29.5% had stage IIB disease, and 41% had stage III disease. Patients also had at least one of the following criteria following radical hysterectomy and pelvic lymph node dissection: lymph node metastasis (39.7%), parametrial invasion (54.4%), and positive resection margin (5.1%).
- The prescribed dose to the planning target volume was 40 Gy, delivered in 16 fractions to the whole pelvis, with any type of IMRT permitted. Overall, 71 patients also underwent concurrent weekly cisplatin (40 mg/m2 of body surface area for three cycles), and eight received fluorouracil (1000 mg/m2 on days 1-5) with cisplatin (60 mg/m2 for two cycles).
- The primary endpoint was the incidence of acute grade 3 or higher gastrointestinal tract, genitourinary, and hematologic toxic effects during radiotherapy or within 3 months of completing radiotherapy.
TAKEAWAY:
- After radiotherapy, only two patients (2.5%) experienced acute grade 3 or higher toxic effects. One was hospitalized for enterocolitis on the last day of radiotherapy and developed grade 3 anemia 3 months after completing radiotherapy; the other experienced hematologic toxic effects and also developed grade 3 anemia 3 months after completing radiotherapy.
- No patients experienced late grade 3 or higher toxic effects.
- When assessing toxic effects of any grade, acute and late gastrointestinal tract toxicities occurred in 76% and 31.6% of patients, respectively; acute and late genitourinary toxicities, all grade 1, occurred in 19% and 24.1% of patients, respectively; and hematologic toxicities occurred in 29.1% and 6.3% of patients, respectively.
- Overall, at 3 years, 79.3% of patients were disease-free and 98% were alive. After a median follow-up of 43 months, 16 patients (20.3%) experienced disease recurrence, four of whom were salvaged and three of whom died.
IN PRACTICE:
“This nonrandomized controlled trial is the first prospective trial, to our knowledge, to show acceptable acute toxic effects of hypofractionated IMRT for cervical cancer in a postoperative concurrent chemoradiotherapy setting,” the authors said, adding that the rate of grade 3 or higher acute toxic effects of 2.5% reported in this study was “substantially lower than our initial hypothesis of less than 15%.”
However , in an accompanying editorial, Mark E. Bernard, MD, of the University of Kentucky College of Medicine, Lexington, Kentucky, highlighted caveats to the study design and raised two core questions: “Should acute toxic effects be the primary endpoint of a single-group, phase 2 study using hypofractionation with fewer cycles of concurrent chemotherapy? Should the primary endpoint rather have been a cancer control endpoint, such as disease-free survival, overall survival, or local control?”
Still, Bernard wrote, “This trial does help lay the foundation for future pelvic hypofractionated trials with concurrent chemotherapy, especially for gynecological malignant tumors.”
SOURCE:
The research, led by Won Park, MD, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea, was published in JAMA Oncology last month.
LIMITATIONS:
The trial is a single-arm study, with a short follow-up time. In the editorial, Bernard listed several limitations, including the fact that patients received fewer cycles of concurrent chemotherapy than what’s typically given in this population.
DISCLOSURES:
No funding or relevant financial relationships were declared.