Key takeaways:
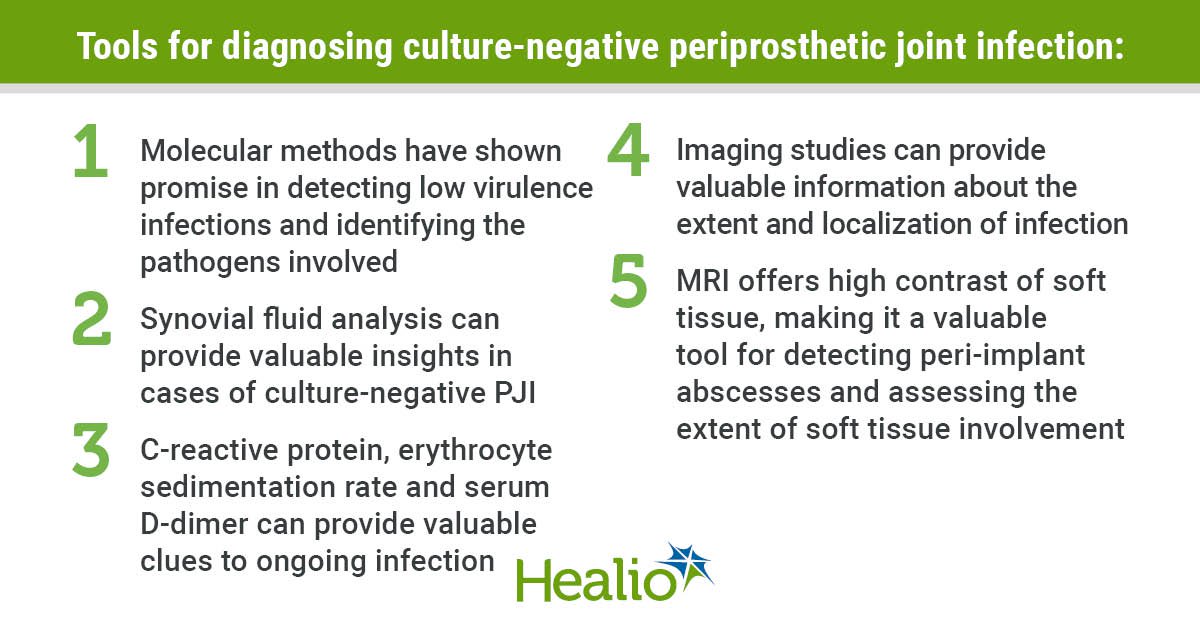
- Synovial fluid analysis can provide valuable insights in cases of culture-negative periprosthetic joint infection.
- Imaging studies can provide valuable information about the extent and localization of infection.
Periprosthetic joint infection remains one of the most dreaded complications following joint arthroplasty.
Traditionally, diagnosing PJI has relied heavily on the culture of microorganisms from synovial fluid or tissue samples. However, a significant challenge exists in cases where these cultures return with negative results. Culture-negative PJI is a perplexing issue, often requiring a multifaceted approach to diagnose and treat. This Infection Watch aims to shed light on the complexities of culture-negative PJI, emphasizing the importance of alternative diagnostic methods and the evolving landscape of management.

Image: Alisina Shahi, MD, PhD; Adam Freedhand, MD
Challenges in diagnosis
Culture-negative PJI poses a substantial diagnostic challenge for orthopedic surgeons and infectious disease specialists. The absence of positive cultures can result from prior antibiotic therapy, low bacterial load or biofilm formation, making it difficult to identify the causative microorganism. Such cases may lead to delayed or inappropriate treatment, increasing the risk of chronic infection, failure and subsequent revision surgery.

Alisina Shahi
Given the limitations of traditional culture-based methods, alternative diagnostic techniques have emerged as crucial tools in managing culture-negative PJI. Molecular methods, including polymerase chain reaction and next-generation sequencing (NGS), have shown promise in detecting low virulence infections and identifying the pathogens involved. These techniques offer faster and more sensitive results, allowing for more timely intervention.
Synovial fluid tests, serological biomarkers
Synovial fluid analysis can provide valuable insights in cases of culture-negative PJI. Leukocyte esterase, an enzyme produced by white blood cells, can be elevated in the presence of infection. In addition, alpha defensin, a small antimicrobial peptide, has gained attention as a specific marker for PJI. Studies have shown that synovial alpha defensin has high sensitivity and specificity, making it a valuable tool for diagnosing PJI, especially in culture-negative cases.
Serological biomarkers like C-reactive protein, erythrocyte sedimentation rate and serum D-dimer remain essential in the evaluation of culture-negative PJI. Elevated levels of these markers can provide valuable clues to ongoing infection. However, it is important to note that these indicators are nonspecific and can be influenced by various factors. Furthermore, these tests do not provide guidance for antibiotic selection. Combining serological biomarkers with other diagnostic methods improves diagnostic accuracy.
Imaging modalities
Imaging studies, such as fluorodeoxyglucose-positron emission tomography and white blood cell scintigraphy, can provide valuable information about the extent and localization of infection. In culture-negative cases, these noninvasive tools are instrumental in guiding surgical interventions and assessing treatment response.
Advanced imaging techniques, such as MRI and ultrasound, have shown promise in the evaluation of culture-negative PJI. In particular, MRI offers high contrast of soft tissues, making it a valuable tool for detecting peri-implant abscesses and assessing the extent of soft tissue involvement.
Management of culture-negative PJI
Once diagnosed, managing culture-negative PJI requires a tailored approach. A multidisciplinary team that includes orthopedic surgeons and infectious disease specialists is essential for guiding proper treatment decisions.
The two-stage exchange is a treatment option that involves a staged approach to address culture-negative PJI. In the first stage, the infected prosthesis is removed and a temporary antibiotic spacer is placed. The patient then undergoes a course of antimicrobial therapy. This approach ensures that the infection is eradicated before a new implant is introduced, reducing the risk of recurrent infection. The second stage involves re-implantation of a new prosthesis once the infection is eradicated.
Conclusion
Culture-negative PJI presents a considerable challenge in orthopedic practice. Timely and accurate diagnosis is essential for guiding appropriate treatment decisions. While traditional culture-based methods have limitations, molecular diagnostic techniques such as NGS; synovial tests like leukocyte esterase and alpha defensin; imaging modalities; and serological biomarkers, including serum D-dimer, are invaluable tools for diagnosing culture-negative PJI. Once the diagnosis of PJI has been made, targeted treatment can begin based on the clinical circumstances.
References:
- Alijanipour P, et al. Clin Orthop Relat Res. 2013;doi:10.1007/s11999-013-3070-z.
- Ko LM, et al. Orthop Clin North Am. 2016;doi10.1016/j.ocl.2015.08.003.
- Romanò CL, et al. J Clin Med. 2020;doi:10.3390/jcm9082548.
- Verberne SJ, et al. J Bone Joint Surg Am. 2016;doi:10.2106/JBJS.15.00898.
For more information:
Adam M. Freedhand, MD, can be reached at 950 Corbindale Road, Suite 300, Houston, TX 77024; email: adam.m.freedhand@uth.tmc.edu.
Alisina Shahi, MD, PhD, can be reached at 7000 Fannin St., Houston, TX 77030; email: alisinair@gmail.com.