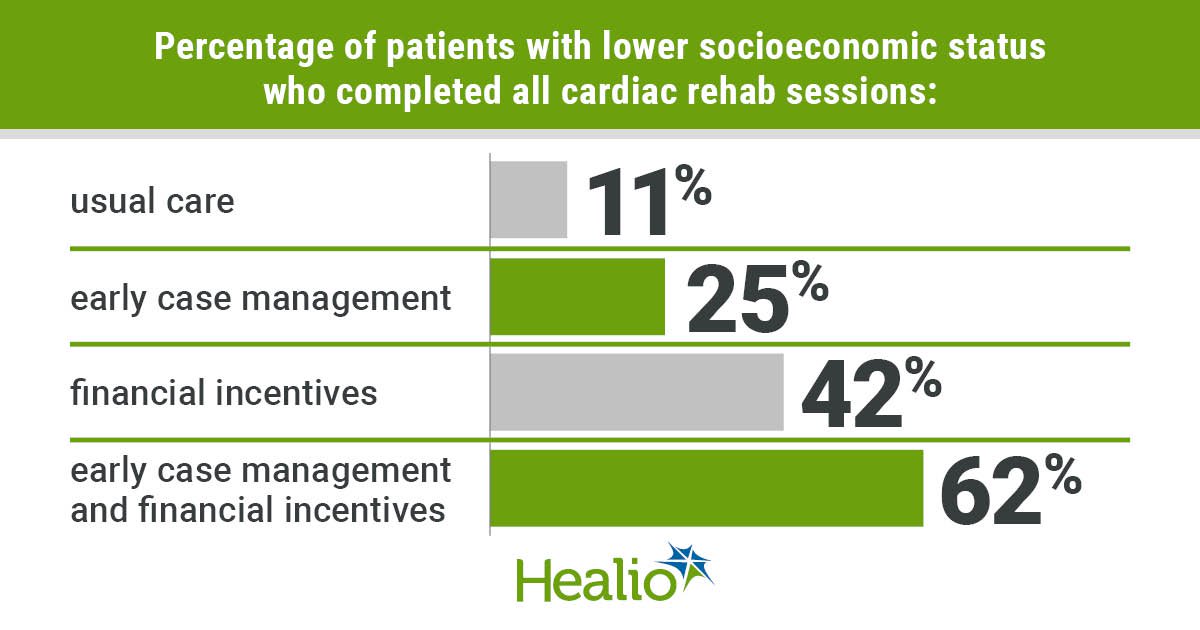
Key takeaways:
- Early case management and financial incentives increased cardiac rehab participation for patients with lower socioeconomic status.
- The greatest effect occurred for patients assigned both interventions.
ATLANTA — Among patients with lower socioeconomic status, interventions based on case management and financial incentives improved attendance at cardiac rehabilitation sessions, according to the results of the HeLP trial.
“When you look at our patients with lower socioeconomic status, they have higher risk factors across the board,” Diann Gaalema, PhD, researcher and assistant professor of medicine at the University of Texas Medical Branch, who was with the University of Vermont Medical Center at the time the study was conducted, said during a presentation at the American College of Cardiology Scientific Session. “Across every single risk factor that we examined, the lower [socioeconomic status] patients are significantly more likely to have those risk factors. And [in] current smoking and depressive symptoms, it’s especially disparate. Given these higher risk factor profiles, it shouldn’t be any surprise that these patients develop their cardiovascular disease more quickly, and they also have worse outcomes after they have these cardiac events.”

Data were derived from Gaalema D, et al. Featured clinical research II. Presented at: American College of Cardiology Scientific Session; April 6-8, 2024; Atlanta.
She said one study has shown that patients with lower socioeconomic status (SES) have elevated risk for mortality after cardiac events compared with other patients, but that much of the excess could be attributed to differences in risk factors, which are manageable through interventions.
Importance of cardiac rehab
One way of intervening is getting these patients to go to cardiac rehabilitation after cardiac events, as that is associated with better long-term outcomes, she said.
“These programs are focused on structured, progressive exercise that rebuilds the cardiovascular system, along with counseling and education to address these other risk factors,” Gaalema said. “It shouldn’t be surprising that attending cardiac rehab is associated with improvements in morbidity and mortality. Unfortunately, [cardiac rehab attendance] is exceptionally low [in] our lower SES patients, even independent of direct financial factors such as insurance coverage. The aim of this trial was to improve cardiac rehab attendance among these lower SES patients, and our primary aim was to test the efficacy of patient-facing incentives and early case management.”
The case management intervention consisted of a brief in-person hospital visit and in-depth needs assessment and setting of goals after discharge, weekly phone calls for 16 weeks and the availability of a case manager by phone for acute need. The financial incentive intervention consisted of receiving money for each cardiac rehab session, starting at $20 for the first session and increasing by $2 for each session thereafter (capping at $40).
The researchers randomly assigned 192 patients from University of Vermont Medical Center who qualified for cardiac rehab and had low SES (mean age, 58 years; 35% women; 44.3% current smokers; 23.7% with moderate or severe depression) on a 2:3:3:3 basis to the usual care, case management only, financial incentives only or case management and financial incentives. Patients were followed for approximately 1 year.
Among the cohort, 56.3% had PCI, 15.1% had CABG, 11.5% had valve replacement or repair, 10.9% had chronic systolic HF, 4.7% had MI and 1.6% had stable angina, according to the presentation.
Benefit of interventions
The percentage of patients completing all 30 cardiac rehab sessions was lowest in the usual care group and highest in the case management/financial incentives group (usual care, 11%; case management, 25%; financial incentives, 42%; case management/financial incentives, 62%; P for trend < .001), according to the researchers.
Among patients receiving the case management intervention, 93% completed the initial needs assessment and 71% of weekly calls were completed, whereas for those receiving the financial incentive intervention, 82% earned at least some of the financial incentives, with an average of $670 earned, Gaalema said.
“It’s encouraging to see … that with interventions, we can improve [cardiac rehab] attendance in this population,” Gaalema said during the presentation. “The next step … is to do a larger trial where we are powered to look at health outcomes as a result of our interventions.”