NEW ORLEANS — Adrenalectomy for the treatment of mild autonomous cortisol secretion (MACS) appears to improve bone quality but not bone density, new data suggested.
Formerly called “subclinical Cushing Syndrome,” MACS is the name now used when a patient with an incidentally discovered adrenal mass has no overt Cushing symptoms but has cortisol levels greater than 1.8 mcg/dL after a dexamethasone suppression test and adrenocorticotropic hormone (ACTH)-independence is confirmed.
People with MACS are at increased fracture risk, and prior studies have suggested that this risk is independent of bone density loss and primarily due to impaired bone quality, study author Jasmine Saini, MBBS, a research fellow at the Mayo Clinic, Rochester, Minnesota, said at the annual meeting of the American Association of Clinical Endocrinology.
She presented the findings of a new study of 41 patients with MACS and 31 reference individuals in which treatment of MACS with adrenalectomy appeared to improve bone quality as assessed by trabecular bone score (TBS) without affecting bone density.
“Considering that improvement in TBS was not mirrored by improvement in bone density, our findings suggest that MACS impacts bone quality more than bone density, and bone density may not identify patients at risk for fractures due to MACS. As TBS is a clinically available test, our findings suggest that clinicians should consider obtaining TBS in addition to bone density when evaluating patients with MACS and when assessing response to therapy,” Saini told Medscape Medical News.
Session moderator Anupam Kotwal, MD, assistant professor in the Division of Diabetes, Endocrinology & Metabolism, at the University of Nebraska Medical Center, Omaha, told Medscape Medical News, “The trabecular bone score being low has been linked with fracture risk, but it does have to be used in conjunction with the bone density. We don’t know what that does in someone with normal bone density if they have a slightly low TBS.”
Kotwal added, “These are markers. The endpoint is fracture reduction rate, and that will require a much longer study with much larger numbers. So, we use bone density as a surrogate…I think TBS by itself is a useful marker in conditions where the traditional factors that affect bone density are not the only ones at play. And we know high cortisol does affect bone density.”
Regarding the use of adrenalectomy to treat MACS, Kotwal noted that surgery is usually reserved for cases with complications or very large nodules. “Just mildly high cortisol and a small adrenal mass — usually you would monitor it and not remove it.”
Indeed, Saini told Medscape Medical News, “The decision is based on the comorbidities, such as having uncontrolled hypertension on three drugs or diabetes that’s not controlled. The surgery may help with metabolic outcomes. It’s a very individualized approach even with the guidelines…However, at Mayo, usually most patients are referred from other centers so there is a referral bias of sending these patients for surgery.”
The guidelines she referenced, from Europe, do leave room for clinical judgement. They recommend adrenalectomy as the standard of care for unilateral adrenal tumors with clinically significant hormone excess. But, in the case of MACS, surgery “can be considered in patients with relevant comorbidities, taking into account individual factors.” And, they recommend against surgery in patients with an asymptomatic, nonfunctioning unilateral adrenal mass and obvious benign features on imaging studies.”
Adrenalectomy Improves Bone Quality, Not Density
The single-center prospective cohort study enrolled adults with MACS who were scheduled for adrenalectomy participants between April 2018 and August 2023 from Mayo Clinic’s Endocrine Outpatient Department. They were matched by age and sex with healthy referent subjects.
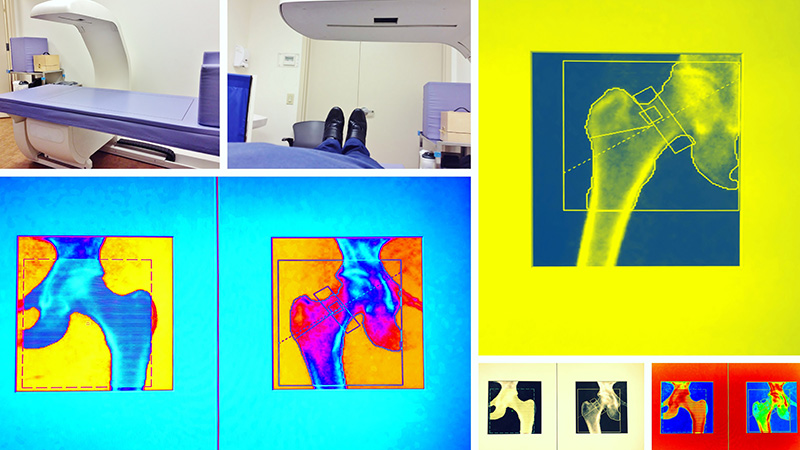
All participants underwent a bone density scan with TBS at baseline and a follow-up evaluation at least 10 months later, with a mean of 1.6 years.
After adrenalectomy, there were no differences between the patients with MACS and the referent subjects in terms of total femur, femur neck, or spine L1-L4 bone mineral density. Forearm radius density deteriorated significantly in both groups (−0.034g/cm and −0.018g/cm, respectively; both P < .001), with the difference also being significant between the two groups (P < .001). The reason for that loss in both groups isn’t clear but may relate to aging and possible hydrocortisone use in the MACS patients, Saini speculated.
However, spine L1-LT4 TBS scores improved significantly in the MACS group (mean difference, 0.037; P = .015) but not in the referent group (−0.004, P = .644).
Both Saini and Kotwal noted that the lack of a comparison group of conservatively matched MACS patients was a study limitation.
However, Kotwal told Medscape Medical News that if these findings are validated, they could influence treatment decision-making. “If a patient has a bad TBS and not terrible bone density, should they be offered adrenalectomy? I don’t think so just based on this study. But I do think if they extend the number of patients and their outcomes or another center validates [the findings] then that could be an additional factor where these patients could be offered surgery even if they don’t have dyslipidemia or dysglycemia.”
Indeed, Saini concluded in her presentation, “Large-sized prospective or randomized controlled trials with conservatively managed patients with MACS are needed to fully characterize the impact of adrenalectomy on bone density and microarchitecture.”
Her group does plan to conduct a larger prospective study. They’re also recruiting for an intervention trial on the safety and tolerability of metyrapone therapy in patients with MACS.
Saini and Kotwal had no disclosures.
Miriam E. Tucker is a freelance journalist based in the Washington DC area. She is a regular contributor to Medscape, with other work appearing in the Washington Post, NPR’s Shots blog, and Diatribe. She is on X @MiriamETucker.