TOPLINE:
Treatment with biologic disease-modifying antirheumatic drugs (bDMARDs), particularly tocilizumab, can suppress inflammation and preserve renal function in a majority of patients with chronic inflammatory disorders who develop serum amyloid alpha (SAA) amyloidosis.
METHODOLOGY:
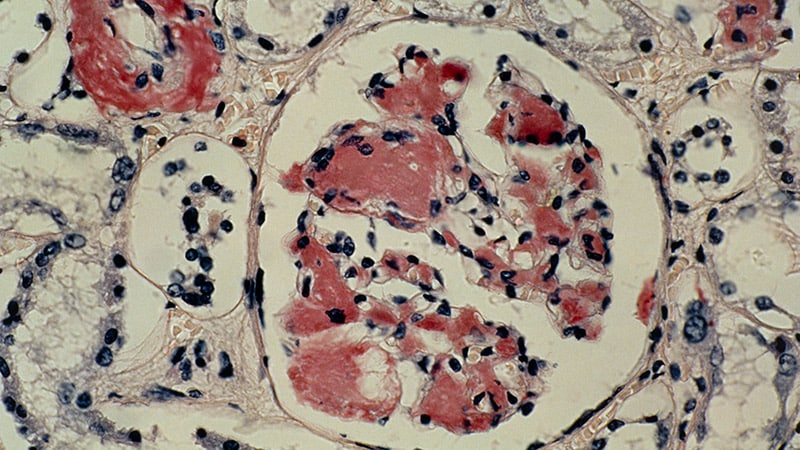
- AA amyloidosis, characterized by the misfolding of the SAA protein, is observed in patients with inflammatory diseases and can lead to progressive organ damage, including chronic kidney disease, malabsorption with cachexia, and cardiac failure.
- This monocentric, retrospective analysis assessed the effect of bDMARD therapy on inflammatory biomarker levels and renal outcomes in 83 patients with AA amyloidosis who were followed for a mean period of 4.82 years.
- The patients were stratified into three major subgroups depending on the cause of AA amyloidosis:
- Chronic inflammatory diseases (cid + AA; n = 34) such as rheumatoid arthritis, Crohn’s disease, and chronic infections
- Autoinflammatory syndromes (auto + AA; n = 24) such as familial Mediterranean fever (FMF) and cryopyrin-associated periodic syndrome (CAPS)
- Idiopathic AA (idio + AA; n = 25), wherein the primary disease could not be identified
- Tocilizumab was the most commonly used bDMARD in patients with cid + AA and idio + AA amyloidosis, and interleukin-1 inhibitors were prescribed to patients with auto + AA amyloidosis because tocilizumab has not been approved yet for FMF or CAPS treatment.
- All patients with AA amyloidosis had renal involvement, as confirmed by kidney biopsy.
TAKEAWAY:
- After bDMARD therapy, C-reactive protein levels reduced significantly from baseline to the last-documented visit in all subgroups, while SAA levels declined in the subgroups cid + AA and idio + AA and proteinuria dropped in the subgroups auto + AA and idio + AA.
- bDMARDs prevented progression to end-stage renal disease (ESRD) in 75% of the patients in the overall cohort, with progression to ESRD being prevented in 60% of patients with cid + AA, 88% of patients with auto + AA, and 81% of patients with idio + AA.
- Tocilizumab was more effective than other bDMARDs in preventing renal progression to ESRD (P = .0006), with a similar pattern observed for the subgroups cid + AA (P = .0126) and idio + AA (P = .0259).
- None of the patients receiving tocilizumab died during the nearly 5-year follow-up period.
IN PRACTICE:
“The data suggest preferential use of IL [interleukin]-1 inhibitors and tocilizumab for clinical use in the treatment of AA amyloidosis depending on the respective underlying diseases,” the authors commented.
SOURCE:
This study, led by Peter Kvacskay, MD, of Heidelberg University Hospital, Heidelberg, Germany, was published online on April 23 in Annals of the Rheumatic Diseases.
LIMITATIONS:
Authors acknowledged the retrospective nature of the analysis and missing data of single patients during the long-term follow-up as major limitations. Furthermore, the cid + AA subgroup was heterogeneous in terms of the pathophysiology of their underlying primary disease.
DISCLOSURES:
This study did not report any source of funding. The authors declared no conflicts of interest.